Table of Contents
What is Diabetic Ketoacidosis (DKA)?
Diabetic Ketoacidosis, commonly known as DKA, is a serious and life-threatening emergency that mainly affects people with diabetes, especially Type 1 diabetes, though it can also occur in Type 2 diabetes under certain conditions.
In simple words, DKA happens when the body does not have enough insulin. Because of this insulin shortage, glucose (sugar) cannot enter the body’s cells to be used as energy. This means that instead of using glucose for energy, the body begins to break down fat. This fat breakdown produces acidic substances called ketones.
When ketones build up in large amounts, they make the blood acidic, leading to diabetic ketoacidosis. If not treated on time, diabetic ketoacidosis can progress rapidly and may lead to coma or death.
DKA is not just “high sugar.” It is a combination of three dangerous problems:
- High blood glucose
- Ketone accumulation
- Metabolic acidosis
Because of its rapid progression and high mortality risk, diabetic ketoacidosis is considered a medical emergency requiring immediate hospital care.
Pathophysiology of Diabetic Ketoacidosis
Understanding the pathophysiology of DKA helps both doctors and patients appreciate why early treatment is critical.
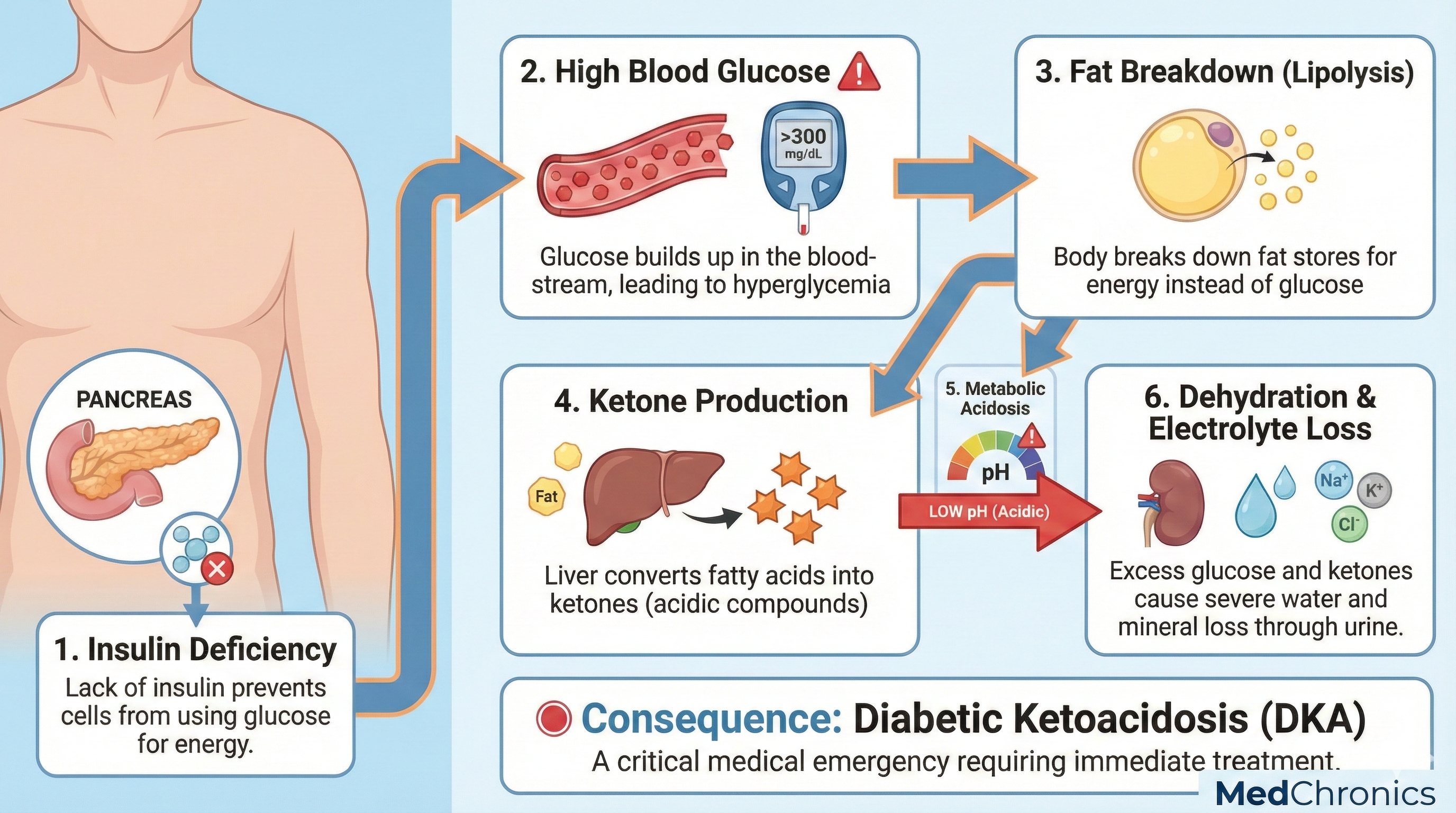
Step 1: Absolute or Relative Insulin Deficiency
- Insulin is required for glucose to enter cells.
- In DKA, insulin is either absent (Type 1 diabetes) or insufficient (Type 2 diabetes during stress, infection, or insulin omission).
Step 2: Increased Counter-Regulatory Hormones
Because insulin is low, the body releases stress hormones:
- Glucagon
- Cortisol
- Catecholamines (adrenaline)
- Growth hormone
These hormones increase blood glucose levels by:
- Stimulating gluconeogenesis (new glucose formation)
- Increasing glycogen breakdown
Step 3: Hyperglycaemia and Osmotic Diuresis
- Blood glucose rises sharply.
- Excess glucose spills into urine.
- Water and electrolytes are lost through urine (osmotic diuresis).
This causes:
- Severe dehydration
- Loss of sodium, potassium, chloride, phosphate
Step 4: Lipolysis and Ketogenesis
- Due to lack of insulin, fat breakdown (lipolysis) increases.
- The liver breaks down free fatty acids into ketone bodies:
- Beta-hydroxybutyrate
- Acetone
- Acetoacetate
Step 5: Metabolic Acidosis
- Ketones are acidic.
- Their accumulation lowers blood pH.
- This leads to high anion gap metabolic acidosis.
Step 6: Electrolyte Shifts
- Potassium moves out of cells into the blood (appearing normal or high initially).
- Total body potassium is actually severely depleted.
- Once insulin therapy starts, potassium shifts back into cells, causing hypokalaemia if not corrected.
This entire process explains why diabetic ketoacidosis (DKA) is complex and why treatment must be carefully monitored.
Causes of Diabetic Ketoacidosis
1. Type 1 Diabetes
- The most common cause
- New onset Type 1 diabetes may present first time as diabetic ketoacidosis (DKA).
2. Insulin Omission or Inadequate Insulin
- Skipping insulin doses
- Poor compliance
- Faulty insulin pumps
- Financial or access issues
3. Infections
- Pneumonia
- Urinary tract infection
- Sepsis
- Skin infections
Infections increase insulin demand and trigger DKA.
4. Acute Medical Conditions
- Myocardial infarction
- Stroke
- Pancreatitis
- Trauma or surgery
5. Drugs and Substances
- Corticosteroids
- Thiazide diuretics
- Sympathomimetics
- SGLT-2 inhibitors (can cause euglycaemic DKA)
6. Stress and Pregnancy
- Physical or emotional stress
- Pregnancy increases insulin resistance
Signs & Symptoms of Diabetic Ketoacidosis
1- Early Symptoms
- Excessive thirst (polydipsia)
- Frequent urination (polyuria)
- Fatigue and weakness, dry mouth
2- Gastrointestinal Symptoms
- Nausea
- Vomiting
- Abdominal pain (common in children)
3- Respiratory Symptoms
- Deep, rapid breathing (Kussmaul respiration)
- Shortness of breath
4- Neurological Symptoms
- Confusion
- Drowsiness
- Altered consciousness
- Coma (severe cases)
5- Classic Warning Signs
- Fruity or acetone-like breath
- Severe dehydration
- Low blood pressure
- Rapid heart rate
Any diabetic patient with vomiting, abdominal pain, and fast breathing should be evaluated immediately for Diabetic Ketoacidosis (DKA).
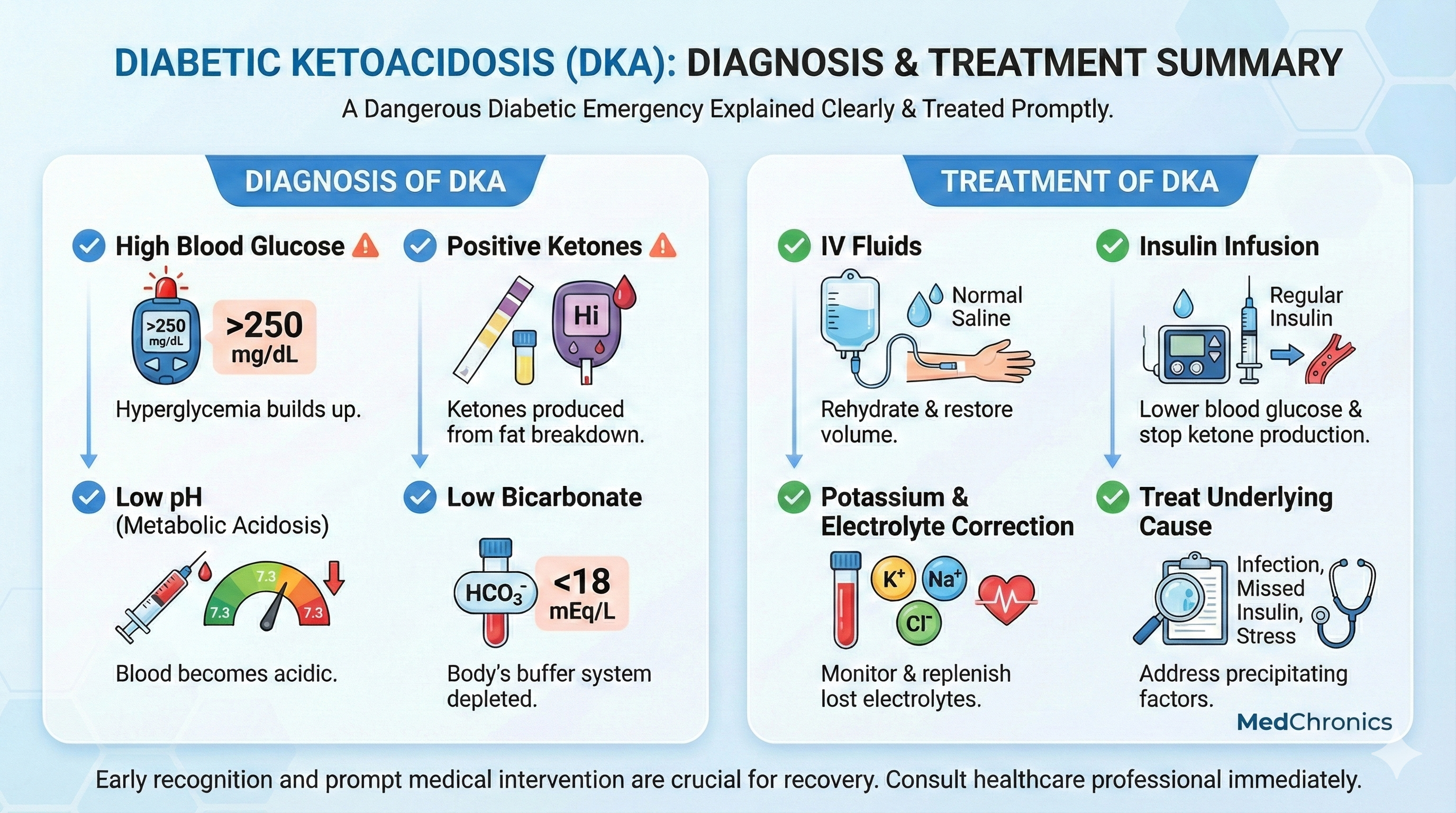
Diagnosis of DKA (ABG, Ketones, Glucose)
Laboratory results with clinical characteristics are used to make the diagnosis.
Diagnostic Criteria
Diabetic Ketoacidosis (DKA) is diagnosed when all three are present:
1- Hyperglycaemia
- Blood glucose > 250 mg/dL
- (May be normal in euglycaemic DKA)
2- Ketonaemia or Ketonuria
- Serum beta-hydroxybutyrate ≥ 3 mmol/L
- Positive urine ketones
3- Metabolic Acidosis
- Arterial pH < 7.30
- Serum bicarbonate < 18 mEq/L
- Increased anion gap
4- Additional Investigations
- Arterial blood gas (ABG)
- Serum electrolytes
- Blood urea and creatinine
- Complete blood count
- Urinalysis
- ECG (for potassium abnormalities)
- Infection workup if indicated
Treatment of Diabetic Ketoacidosis (DKA)
Management of DKA should always be done in a hospital setting, preferably in the ICU for moderate to severe cases.
1. Fluid Replacement (First Priority)
- Start with 0.9% normal saline
- Initial rate: 15–20 mL/kg in the first hour
- Correct dehydration and improve circulation
2. Insulin Therapy
- Regular insulin IV infusion
- Dose: 0.1 units/kg/hour
- Goal: Gradual reduction of glucose (50–75 mg/dL/hour)
Once glucose < 200 mg/dL:
- Add dextrose to fluids
- Continue insulin until acidosis resolves
3. Electrolyte Management
Potassium is critical
- If K⁺ < 3.3 mEq/L → Correct potassium first.
- If K⁺ 3.3–5.2 → Add potassium to fluids.
- Continuous monitoring is essential.
4. Bicarbonate Therapy
- Generally not recommended.
- Consider only if pH < 6.9.
5. Treat Underlying Cause
- Antibiotics for infection.
- Restart or adjust insulin therapy.
- Manage precipitating illness.
6. Monitoring
- Hourly blood glucose.
- Frequent electrolytes and ABG.
- Strict intake–output charting.
Complications of Diabetic Ketoacidosis
Acute Complications
- Cerebral edema (especially in children).
- Hypokalaemia.
- Acute kidney injury.
- Shock.
- Cardiac arrhythmias.
Long-Term Complications
- Recurrent hospitalizations.
- Increased mortality risk.
- Reduced quality of life.
Without timely treatment, Diabetic Ketoacidosis (DKA) can be fatal.
Prevention of Diabetic Ketoacidosis
For Patients
- Never skip insulin doses.
- Monitor blood glucose regularly.
- Check ketones during illness.
- Stay hydrated.
- Seek medical help early.
Sick Day Rules
- Continue insulin even if not eating.
- Increase glucose monitoring.
- Drink fluids frequently.
- Contact the doctor if sugar levels remain high.
For Healthcare Providers
- Patient education.
- Early identification of high-risk individuals.
- Regular follow-up.
Diabetic Ketoacidosis is a medical emergency that demands immediate recognition and prompt treatment. Despite advances in diabetes care, Diabetic Ketoacidosis (DKA) remains a significant cause of morbidity and mortality worldwide. Early diagnosis, guideline-based management, and strong patient education are the keys to reducing its impact.
For patients, understanding warning signs can be life-saving.
For healthcare professionals, strict adherence to protocols ensures better outcomes.
Frequently Asked Questions
Q. Is Diabetic Ketoacidosis (DKA) only seen in Type 1 diabetes?
Mostly yes, but it can also occur in Type 2 diabetes, especially during stress or infections.
Q. Can Diabetic Ketoacidosis (DKA) occur with normal blood sugar?
Yes, this is called euglycaemic DKA, commonly associated with SGLT-2 inhibitors.
Q. How fast does DKA develop?
DKA can develop within 24 hours, sometimes even faster.
Q. Is DKA preventable?
Yes, with proper insulin use, education, and early intervention.
Q. Is DKA life-threatening?
Yes. Without treatment, it can lead to coma or death.